I reached a point in my life where I was constantly tired, burnt out, and wondering what on earth was happening inside my body. No matter how much I rested, I still felt exhausted. I noticed I was more anxious, more irritable, and I wasn’t sleeping the way I used to. It felt like something was off — but I couldn’t quite put my finger on it.
So, I did what many of us would do: I went to my doctor and asked for blood work. I needed answers. What she explained to me was something I had barely even heard of before — perimenopause. And here’s the thing: this is something women should become aware of long before it begins.
The truth is, no one really prepares us for this transition. We hear plenty about puberty, pregnancy, and menopause, but almost nothing about the years in between when our hormones begin to shift. That silence leaves women feeling scared, confused, and unprepared.
That’s why I want to share this post with you — so you feel informed, supported, and ready to navigate this chapter with confidence. In this post, I’ll break down:
What perimenopause actually is
The science of what’s happening inside your body
Why hormone balance is so important
And 14 powerful tips to help you move through perimenopause with ease and grace
Listen to the episode breakdown here:
What is Perimenopause?
Perimenopause is the natural transition before menopause, when your hormone levels start shifting. It can begin anywhere between age 39–44 and typically lasts 3–4 years, but for some women, it can stretch to 8–10 years.
The official end of perimenopause is marked when you’ve gone 12 consecutive months without a period — that’s when you’ve entered menopause.
What’s Really Happening Inside Your Body (and Mind)
Perimenopause isn’t just about physical changes — it’s also about what happens in your brain and nervous system as your hormones shift. When you understand the why, the anxiety, mood swings, and brain fog suddenly make more sense.
Here’s the science, simply explained:
Progesterone Declines First
Progesterone is often called the “calming hormone” because it has a soothing effect on the brain. When it drops, you may feel more anxious, restless, or have trouble sleeping. Without enough progesterone, your body is more sensitive to stress, and fear-based thoughts can feel louder.Estrogen Fluctuates Wildly
Estrogen affects serotonin and dopamine — the “feel-good” neurotransmitters that keep your mood steady and your brain sharp. As estrogen spikes and dips, you may feel sudden waves of sadness, irritability, or brain fog. One day you feel fine, the next you’re exhausted or emotional. It’s not you being “too sensitive” — it’s biology.Cortisol Rises
Cortisol is your stress hormone. Because perimenopause makes your body less resilient to stress, cortisol can become overactive. This is why women in their 40s often notice more overwhelm, intrusive or fearful thoughts, and even panic symptoms. Your nervous system is on higher alert.Sleep Disruption Makes It Worse
As hormones shift, your sleep cycle can become fragmented. Poor sleep then raises cortisol even more, lowers melatonin, and makes anxiety and irritability harder to manage. It becomes a cycle of stress and exhaustion.
✨ Why this matters:
When you recognize that these symptoms are biological, not personal flaws, it changes everything. You realize: “I’m not broken. My hormones are shifting, and I can support my body through this.”
With the right strategies — from protein and strength training to nervous system care and hormone support — you can calm these internal shifts and feel more balanced.
Related Reading: How to create more calm in your life
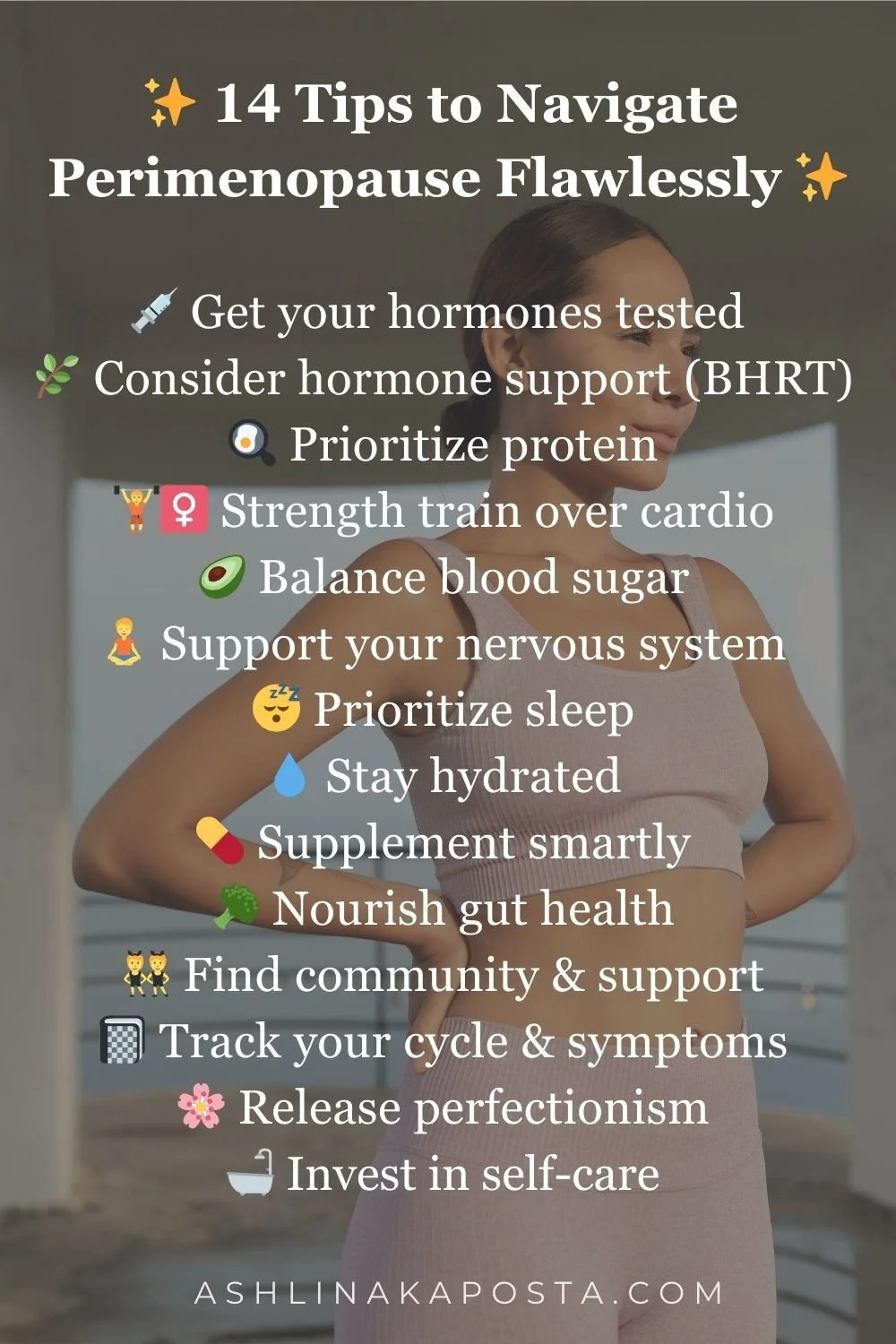
14 Tips to Navigate Perimenopause Flawlessly
Here’s how you can support your body and mind through this season, with science-backed tips and practical takeaways:
💉 1. Get Your Hormones Tested
Ask for a full hormone panel: estrogen, progesterone, testosterone, FSH, LH, thyroid, and cortisol.
Fun fact: Saliva or DUTCH tests often give more accurate hormone fluctuation insights than basic blood work.
Takeaway: Don’t guess — test. Knowledge is the first step to feeling better.
🌿 2. Consider Hormone Support (BHRT)
Bioidentical hormone replacement therapy (BHRT) uses compounds that mimic your body’s natural hormones.
Research shows progesterone can improve sleep, reduce anxiety, and ease night sweats.
Takeaway: Explore options with a women’s hormone specialist — this isn’t one-size-fits-all.
🍳 3. Prioritize Protein
Women over 40 benefit from 1.0–1.2g protein per pound of body weight daily (example: 150 lbs = ~150g).
Protein stabilizes blood sugar, supports muscle, and boosts metabolism.
Takeaway: Build meals around protein — eggs, Greek yogurt, lean meats, legumes, protein powders.
Related Reading: 15 delicious high protein snack ideas for women
🏋️♀️ 4. Strength Train Over Cardio
A Harvard study found women who lifted weights 2–3x per week had better bone density and less belly fat than cardio-only groups.
Muscle loss accelerates after 40 — strength training protects against this.
Takeaway: Aim for 2–3 sessions per week, using weights that challenge you for 8–12 reps.
🥑 5. Balance Blood Sugar
Fluctuating estrogen worsens blood sugar swings.
Tips:
Always pair carbs with protein or fat.
Don’t drink coffee on an empty stomach.
Walk 10 minutes after meals → lowers glucose spikes by 20%+.
Takeaway: Balanced blood sugar = stable mood, weight, and energy.
🧘 6. Support Your Nervous System
High cortisol makes symptoms worse.
Studies show meditation can lower cortisol by 25%.
Takeaway: Try 5 minutes of box breathing, journaling, or meditation daily.
😴 7. Prioritize Sleep
Poor sleep increases ghrelin (hunger hormone) and worsens brain fog.
Tips:
Magnesium glycinate (200–400mg) before bed.
Keep your room cool (68°F or lower).
Stick to consistent bed/wake times.
Takeaway: Protect your sleep like medicine — it resets your hormones.
💧 8. Stay Hydrated
Aim for half your body weight in ounces daily (150 lbs = 75 oz).
Use electrolytes: sodium, potassium, magnesium, especially if sweating.
Takeaway: Hydration reduces fatigue and helps regulate temperature.
💊 9. Supplement Smartly
Top 5 for perimenopause (check with your provider):
Magnesium glycinate → sleep, relaxation
Omega-3s → brain + inflammation
Vitamin D3 + K2 → bones, mood
Collagen → skin + joints
CoQ10 → energy + heart health
Takeaway: Supplements fill gaps, but start with diet + lifestyle.
🥦 10. Nourish Gut Health
Gut bacteria help metabolize estrogen.
Include: fiber (chia, flax), fermented foods (sauerkraut, yogurt), prebiotics (bananas, asparagus).
Takeaway: A healthy gut = calmer hormones + smoother digestion.
👯 11. Find Community & Support
Oxytocin (the bonding hormone) reduces cortisol and eases symptoms.
Studies show women with strong social ties experience fewer menopausal symptoms.
Takeaway: Schedule regular connection — coffee dates, group walks, book clubs. Join my Manifestation Queen Membership
📓 12. Track Your Cycle & Symptoms
Use apps like Clue, or keep a journal.
Tracking reveals patterns → you’ll see triggers and trends.
Takeaway: Awareness helps you advocate for yourself and adjust lifestyle choices.
🌸 13. Release Perfectionism
Perfectionism is linked to higher cortisol and worse sleep.
Takeaway: Midlife isn’t about doing it all — it’s about doing what matters. Simplify routines and give yourself grace.
🛁 14. Invest in Self-Care
Warm baths, skincare, journaling, yoga = oxytocin boosters.
Oxytocin lowers stress hormones and supports emotional balance.
Takeaway: Self-care isn’t indulgence. It’s hormone regulation.
Final Thoughts
Perimenopause is not the end of your vitality — it’s the beginning of a new season. With the right support, knowledge, and lifestyle shifts, you can feel strong, vibrant, and flawless.
If you’re feeling off, foggy, or unlike yourself — you are not broken. You’re evolving. ✨
Frequently Asked Questions About Perimenopause
Q: At what age does perimenopause usually start?
Perimenopause often begins in your early 40s, though some women notice changes as early as their late 30s. On average, it starts between ages 39–44 and lasts until menopause, which usually occurs around 51.
Q: How long does perimenopause last?
It varies from woman to woman. For some, it lasts just a few years. For others, symptoms can stretch 8–10 years. The average duration is 3–4 years.
Q: What’s the difference between perimenopause and menopause?
Perimenopause is the transition period leading up to menopause, when hormones fluctuate and cycles change. Menopause officially begins after you’ve gone 12 months without a period.
Q: Can you get pregnant during perimenopause?
Yes. Ovulation becomes less predictable, but pregnancy is still possible until you’ve reached full menopause.
Q: What are the first signs of perimenopause?
Many women first notice changes in their periods — either lighter, heavier, shorter, or longer. Other common early symptoms include brain fog, sleep issues, mood swings, and increased fatigue.
Q: Do all women need hormone therapy?
No. Some women manage symptoms through lifestyle changes alone. Others find hormone therapy life-changing. The best path is individual and should be guided by a qualified women’s health provider.
Q: What foods are best for perimenopause?
Focus on protein-rich foods, leafy greens, fiber, and healthy fats (like avocado and olive oil). Limiting sugar and processed carbs can help stabilize mood and energy.
Q: How can I manage weight gain during perimenopause?
Prioritize protein, strength training, and blood sugar balance. Managing stress and sleep also plays a huge role in weight management during this stage.